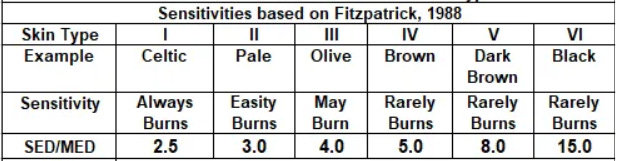
A table in my recent post about the time for skin damage by UV for different skin included the clipping below, which implies that the sensitivity of white skin to UV damage is between 5 and 7.5 times greater than for black skin.
The numbers there are based on the UV doses required to produce the first signs of skin reddening (called ‘erythema’) 24 hours after exposure. There’s a wide range in those in the literature - especially for darker skin types where it’s probably much harder to detect erythema. The comparison between skin types therefore needs to be taken with as grain of salt.
But that sort of skin damage may have nothing to do with the more serious issue of skin cancer -particularly melanoma.
My colleague David Whiteman in Brisbane drew my attention to a couple of relevant papers that I hadn’t seen before about UV effects on different skin type. The work was carried out by a group at Kings College, London, that’s led by another colleague, Antony Young.
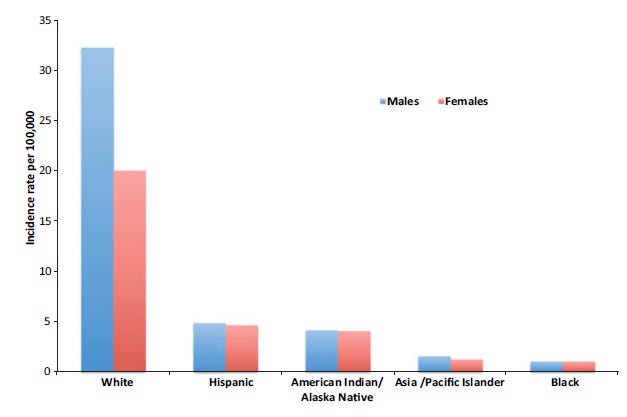
The first paper, published in 2016, includes the figure below that compare the incidence rate of melanoma by ethnicity in the USA.
It shows that the risk for white males is about 20 times greater than for black males (and about 15 times greater for white females than black females). A much larger difference than implied by differences in skin-sensitivities shown in my table. Of course, differences in exposure between skin types may also be important.
The same paper then goes on to describe experiments involving DNA damage rather than skin reddening as an end point. As well as being much more relevant for skin cancer, it’s measurement is also much more objective. The idea is that the melanin in darker skin blocks the UV before damage can occur. So far, so good.
But the paper then makes the statement “DNA photo-damage initiates non-melanoma skin cancer and is reduced by a factor of about 3 in pigmented skin compared with white skin”, and concludes that “regular use of a low sun protection factor sunscreen or other photo-protection strategies (equivalent to melanin photo-protection – dose reduction factor of 3–6), preferably from an early age, would be very beneficial.”
It all seems rather odd. That ratio between blacks and whites is much smaller than implied by the different skin sensitivities for erythema. Yet the ratio in incidence rates, shown by the plot above, is much larger.
A later paper from the same group, published in 2018, muddies the water even more. Even these [slightly edited] sentences in the abstract of the paper seem a bit contradictory.
Melanin in black skin protected against DNA damage by 8.0-fold in the overall epidermis and by 59.0-, 16.5-, and 5.0-fold in the basal, middle, and upper epidermis, respectively. Protection was related to the distribution of melanin, which was most concentrated in the basal layer of black skin. These results may explain, at least in part, the considerable skin color differences in keratincyte cancer (KC) incidence. These data suggest that a DNA protection factor of at least 60 is necessary in sunscreens to reduce white skin KC incidence to a level that is comparable with that of black skin.
There seems to be a mismatch between that and the ‘factor of 8’ or ‘factor of 60’ mentioned in the abstract. Though, with different combinations of those three skin layer factors, either of those factors (8, or 60) could just be possible.
Using DNA damage as a marker does seem a step in the right direction. But there must be something else that I haven’t quite grasped because the numbers don’t add up (I’m only an atmospheric physicist). Any ideas that help resolve this for me would be greatly appreciated because it may affect the advice given in our smartphone apps.
I understand there will be a session on this at a meeting I’ll be attending later this year. I wait with bated breath.



Hi Richard. For me, the key point is where the (DNA) damage happens and what the consequences are at that skin layer. My understanding is that melanoma originates in melanocytes in the basal layer and therefore the ~60 fold protection that darker skin affords to DNA damage in the basal layer is relevant to melanoma occurrence.
While something like SCC, which initiates above the basal (melanocyte) layer, benefits less from the protection that darker skin provides (below in the basal layer) and therefore the rates will be more similar to those in lighter skinned folk. Presumably this will apply to other forms of skin damage, reddening etc depending on where they occur.
To shift into your world, melanin is like having the ozone layer in the basal layer of your skin (which is fine for protecting that layer and those below it, but doesn't really help the layers above), while sunscreen enables you to put your ozone on the outside and protect all skin layers.
Most things in evolution are a compromise. It's interesting that the very melanocyte cells that protect our skin are the same ones that develop into something life-threatening. Presumably a melanin-rich melanocyte is well protected while a 'pale' melanocyte is much more sensitive to damage?
And then of course there's the risk x consequence trade off. Melanoma protection is probably under much greater selective pressure than SCC protection or getting wrinkles, but apparently vitamin D production trumps everything as latitude increases.
Nick King
Hi,I suggest you log onto ‘The difference between Collagen 1 ; 2; and 3”
Collagen makes up about 30% of the body and collagen 1 makes up about 90% of all 5 types.
The skin is made up of three layers—Epidermis ; Dermis and Hypo dermis with the dermis consisting of collagen.
Younger skin dermis is collagen 1 which is synthesised to form very stron cross linked flexible fibrils
As one ages dead collagen 1 cells are replaced with inflexible collagen 3 . From about age 20 the Collagen 1 to 3 ratio changes at a rate of about 1% per year and the result is quite a dramatic change in the collagen structure in the dermis layer leading to wrinkles and less flexibility and sagging skin.
The drivers of this change are due to the turning off of genes Coli 1A1 and Col1A2 for Collagen 1 synthesis with Col 3A1 synthesising Collagen 3 replacement. The relentless structural weakness change of the sheet like soft tissues makes them (as well as other collagen tissues like tendons and blood vessel tissue more prone to injury such as tendonitis and aneurysm in blood vessels from high blood pressure)
The penetration of UV Radiation through the epidermis could easily damage the Demi’s layer of collage and with the capillary blood vessels located between the dermis layer of the skin and the hypo dermis layer which consists of hyaluronan and water then one would expect the skin to turn red possibly due to micro tears
Maybe this helps
Stan R