I recently stumbled across a review paper (as yet not formally published) suggesting that light from artificial lamps like those used in sunbeds is more beneficial than sunlight for maintaining optimal levels of vitamin D. The author reached that conclusion because studies with artificial lamps typically gave larger increases in vitamin D than those involving exposure to natural sunlight. But were the exposures in those studies truly comparable?
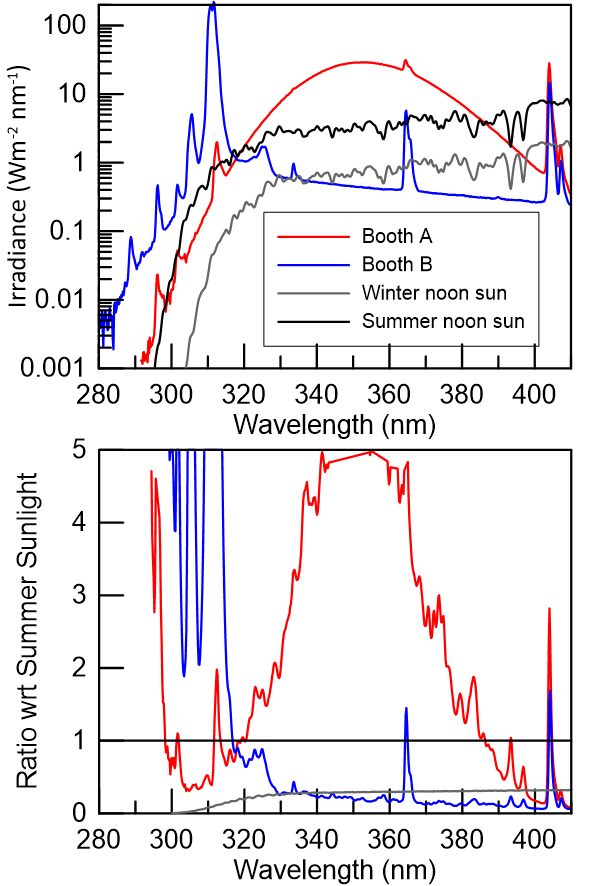
A few years ago, we were part of a study that included making the relevant spectral comparisons. They are shown in plot below (which is similar to one discussed in a recent post). The purpose of the study was to see how much vitamin D was made from exposure to a specialist therapeutic lamp in a dermatological clinic (the blue curve), compared with that produced from exposure to a normal sunbed (the red curve), which was intended as a control. The experiment designers had assumed the sunbed wouldn’t produce any vitamin D. But it did. They were puzzled and asked for our help to explain why.
When you compare the lamp spectra with the spectra from sunlight (black and grey curves) it’s not surprising that both lamps are efficient at producing vitamin D.
As with most spectral plots involving UV wavelengths, it’s plotted on a log scale for the y-axis so you can more clearly see what’s happening at the shortest wavelengths that we’re most interested in here. The sharp peaks that appear in both of the artificial lamps are due to emissions by mercury. The smaller dips in the sun spectra are due to absorptions in the sun’s atmosphere - they’re called Fraunhofer lines.
But that log scale does add a complication for non-mathematicians. To simplify a comparison between the 4 light sources, I’ve plotted the ratios of their spectral output with respect to summer noon sunlight in the lower panel (with the y-axis clipped to a maximum of 5).
As you can see from the plot, compared with sunlight, both artificial sources emit more of the shorter UVB wavelength radiation (less than 313 nm). There’s disagreement in the literature about which wavelengths are most effective in the formation of vitamin D, though there is agreement that they will be at wavelengths less than 313 nm. But similar short wavelengths are also involved in skin damage. So you risk skin damage while satisfying your vitamin D needs (as you do in sunlight, but at least our bodies will have evolved over time to adapt to that). I certainly wouldn’t want people to deliberately expose themselves to either of them without medical supervision.
The peak skin-wrinkling UVA radiation from the sunbed (red) is 5 times larger than in sunlight, and the total UVA is larger by a factor of three. For this lamp, the amount of sunburning UV produced is around UVI = 15 (I’ve seen examples of similar sunbeds with UVI as high as 21). That’s more than for summer sunlight at most places in the world. The recommended exposure times - of around 20 to 30 minutes - are therefore long enough for skin damage to occur, including probable long-term skin-wrinkling from those unnaturally large amounts of UVA. Also (see table below), because the UVI is greater for the lamp, while the vitamin D generated is less, that means that to achieve a given increase in vitamin D, the risk to your skin in exposing yourself to the sunbed is higher than for sunlight (assuming the same attire). If you’re worried about your levels of vitamin D, don’t try using a sunbed to fix the problem. You’d be much better advised to take a supplement. Much cheaper too.
The therapeutic lamp (blue curve) is even more dangerous and should be used only under strict clinical control. You can see that near 312 nm, its output is about 90 times brighter than summer sunlight (the version of the plot displayed is clipped to a maximum value of 5). The recommended exposure times for that lamp are less than one minute.
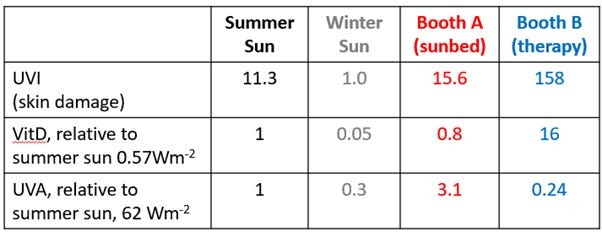
In the Table, I include some relevant comparisons for the four light sources shown in the graph. But note that the relative amounts of vitamin D might change. They assume the currently accepted action spectrum for its production, which is under review. For example, if, as has been suggested, the action spectrum is moved to shorter wavelengths by about 5 nm, then the relative amount produced by booth A relative to sunlight could increase significantly.
Real-life exposure to harmful radiation at the shorter wavelengths is generally much lower from sunlight than for both of those recommended sunbed exposures.
There aren’t many studies relating vitamin D to the exposure to natural sunlight. Most presume (erroneously) that the amount of sunlight people receive is proportional to the amount available. We were involved with one of the very few studies that showed the error in that assumption. Around 500 participants wore personal UV-sensitive badges for several weeks that recorded the UV dose they’d received. Logs were also kept of the clothing, which was used to calculate the fraction of skin exposed. It was typically less than 30 percent. But the dose received would be much larger in summer if more skin were exposed, and lower in winter if less skin is exposed.
We found that on average, participants received less than 3 percent of the available UV dose. Taking those factors together, for a given UVI, the effective sunburning dose in real life is only 1 percent of that in a sunbed. And the dose for vitamin D would be an even smaller fraction because even shorter wavelengths are involved than for sunburn.
It turns out that with our modern lifestyle, we’re hardly ever outdoors receiving the full dose of sunlight - especially near noon when most of it arrives. Because our received fraction of available UV is so small, behavioural differences (e.g., time spent outside, and clothing) are probably more important than variations in UV with time and place.
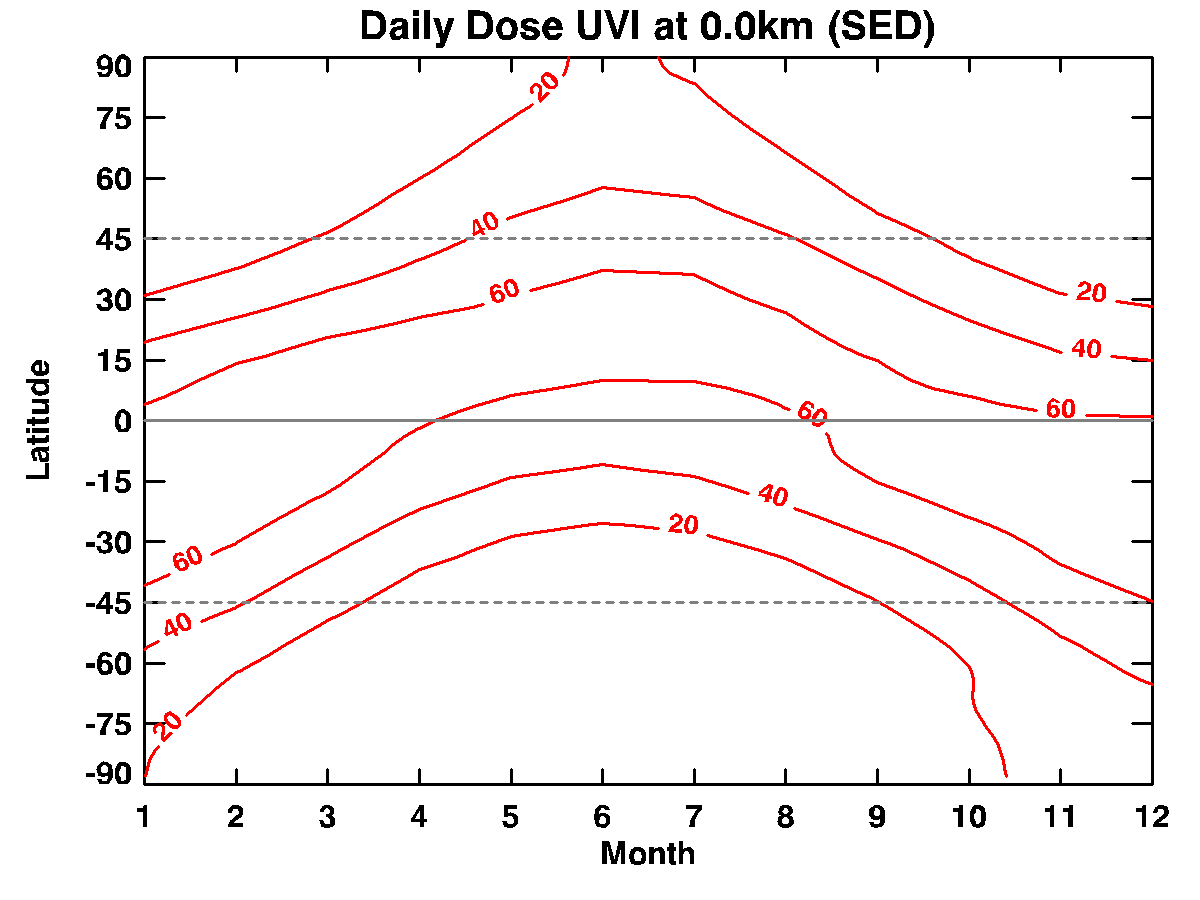
For comparison with sunlight, I dug out this old plot that I made years ago. It shows the calculated available daily dose of sunburning UV from sunlight for clear skies as a function of latitude and month.
The dose is given in SEDs, which stands for “Standard Erythemal Doses”. For fair skin, it takes about 2 SED to induce skin damage - as evidenced by skin-reddening 24 hours after exposure. The plot clearly shows the need for sunscreen-use if you’re outdoors for long periods. As we saw last week, in summer, there can be more than 60 SEDs per day, so even using a sun-screen with a sun protection factor (SPF) of 30, you could still reach a skin damaging dose of 2 SEDs.
For sunburning radiation, the daily dose available at mid-latitudes is usually less than 40 SEDs. But if people receive only 3 percent of that, it’s only around 1 SED. And, because people are generally wearing clothes, that dose is usually received by only a small fraction of their skin area, in contrast to sunbeds where the dose is typically more than 2 SED (and therefore damaging to fair skin), and most of the skin is exposed.
The review isn’t comparing apples with apples.
Of course, we can dream up light sources that are more efficient than sunlight at producing vitamin D. But at what collateral cost to our skin?



Great article Richard, would you be okay if I share this? FYI it has been bought to our attention, a fad promoted on social media, esp amongst teenagers, to follow the UVI and when it reaches peak UV, to then sunbathe until you burn! This is being advised as the fastest way to get a deep tan!! Guess I won’t be out of a job any day soon. Melnet tell us that over 500 people have died in NZ from melanoma and NMSC in the last year but limited public health policy around this. Hope all is well in your neck of the woods and look forward to seeing the team again in August. Cheers Trish